Interference by insurers is driving psychological well being care suppliers to flee networks. It makes remedy exhausting to seek out. Some states are passing legal guidelines to guard sufferers.
Javi Sanz/Getty Photos/E+
conceal caption
toggle caption
Javi Sanz/Getty Photos/E+
Accessing psychological well being care could be a harrowing ordeal. Even when a affected person finds a therapist of their community, their insurance coverage firm can overrule that therapist and resolve the prescribed remedy isn’t medically vital.
This sort of interference is driving psychological well being professionals to flee networks, which makes remedy exhausting to seek out and places sufferers in hurt’s means.
ProPublica sought to know what authorized protections sufferers have towards insurers impeding their psychological well being care.
This story comes from ProPublica, a nonprofit newsroom that investigates abuses of energy. Signal as much as obtain their largest tales as quickly as they’re revealed.
Most Individuals — greater than 164 million of them — have insurance policy by employers. These are usually regulated by federal regulation.
Though the regulation requires insurers to supply the identical entry to psychological well being care as to bodily care, it doesn’t require them to rely on evidence-based tips or these endorsed by skilled societies in figuring out medical necessity. As an alternative, when deciding what to pay for, the federal government permits insurers to set their very own requirements.
“If insurers are allowed to residence bake their very own medical necessity requirements, you may just about guess that they’re going to be contaminated by monetary conflicts of curiosity,” stated California psychotherapist and legal professional Meiram Bendat, who specializes in defending entry to psychological well being remedy.
Federal lawmakers who need to enhance affected person protections might look to their counterparts in states who’re pioneering stronger legal guidelines.
Though these state legal guidelines govern solely plans below state jurisdiction, resembling particular person or small-group insurance policies bought by state marketplaces, specialists instructed ProPublica they might, when enforced, function a mannequin for broader laws.
“States are laboratories for innovation,” stated Lauren Finke, senior director of coverage at The Kennedy Discussion board, a nonprofit that has advocated for state laws that improves entry to psychological well being care. “States can take it ahead and use it for proof of idea, after which that may completely be mirrored on the federal stage.”
ProPublica reporters delved into the legal guidelines in all 50 states to find out how some try to chart new paths to safe psychological well being care entry.
Most of the new protections are solely simply beginning to be enforced, however ProPublica discovered that a couple of states have begun punishing corporations for violations and forcing them into compliance.
Who defines what psychological well being care is critical?
Insurers usually face few limitations on how they outline what sort of psychological well being care is medically vital. They usually create their very own inner requirements as a substitute of counting on ones developed by nonprofit skilled medical societies. These requirements can then be used to problem diagnoses or remedy plans.
“Figuring out the revenue motive that insurers have, it’s actually stunning that federal regulation doesn’t outline medical necessity and require the usage of nonprofit tips to make choices,” stated Bendat, who helped California legislators draft a extra sturdy regulation that handed in 2020, changing into one of many first states to take action.
California’s regulation requires insurers to comply with usually accepted requirements of care for psychological well being and substance use circumstances, forcing them to depend on evidence-based sources that set up standards, resembling nonprofit skilled organizations or peer-reviewed research. The state additionally barred insurers from overlaying solely the remedy of short-term or acute signs, resembling disaster stabilization, as a substitute of the underlying situation, like power melancholy.
Final October, California discovered well being care group Kaiser Permanente in violation of the brand new state regulation and different well being care laws, reaching a settlement with the corporate, which agreed to pay a $50 million fantastic and make $150 million in investments in behavioral well being care. A Kaiser spokesperson stated that the corporate takes full accountability for its efficiency and that it had adopted new tips consistent with the regulation. (Learn their full response.)
A spokesperson for the state’s Division of Managed Well being Care stated the company is auditing insurers and figuring out whether or not their networks provide sufficient suppliers to serve clients and whether or not they ship well timed entry to care.
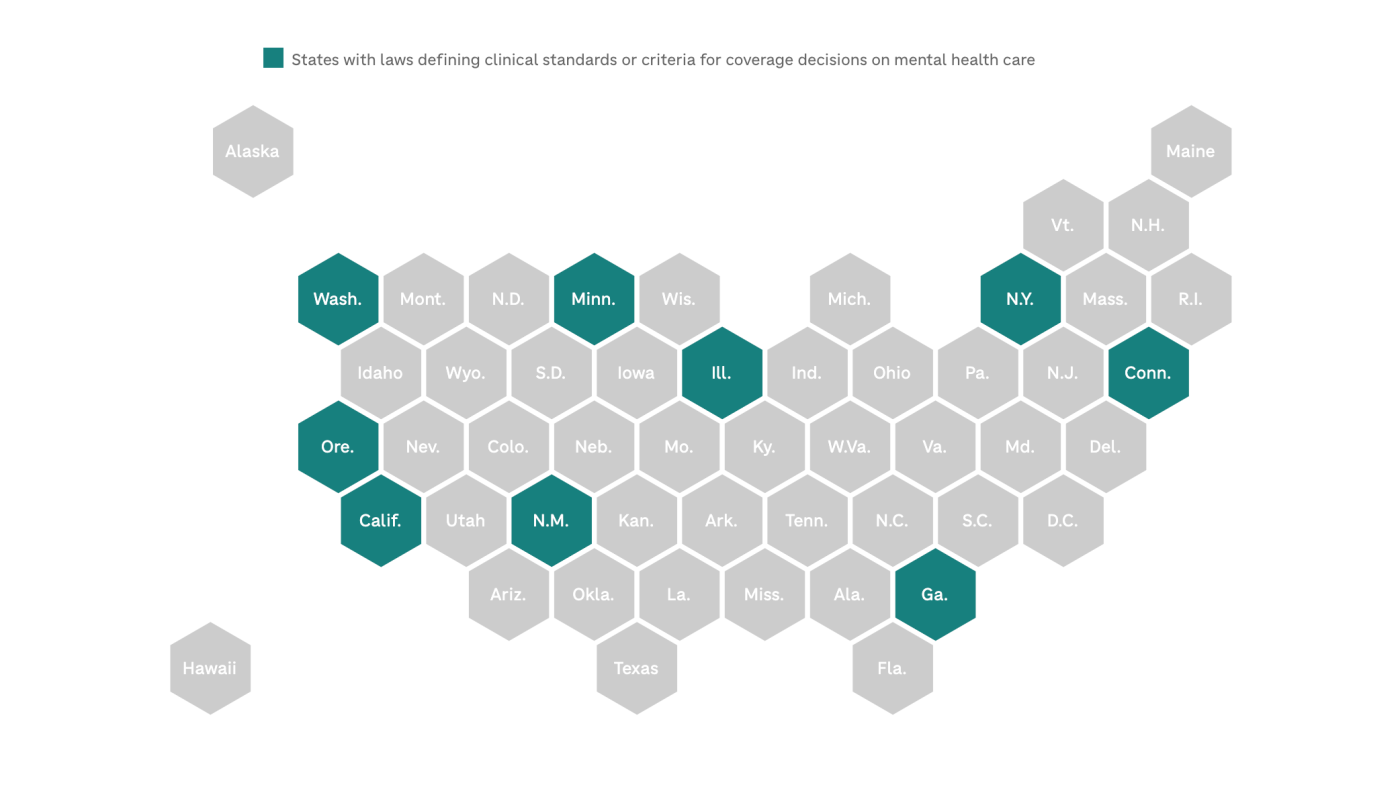
9 states, together with Oregon, Illinois and Georgia, have outlined the scientific requirements or standards that insurers should use when making protection choices on psychological well being care.
Amid the opioid disaster, which has killed greater than one million Individuals, states have additionally instituted medical necessity protections for substance use remedy. For instance, in Colorado, Maryland, Delaware, Connecticut and several other different states, insurers should depend on tips from the American Society of Dependancy Medication when reviewing remedies for substance use.
How can insurers problem psychological well being remedy?
Earlier than 2008, insurance coverage corporations nationwide might put extra stringent limits on how usually sufferers obtained psychological well being care in contrast with medical care, instituting extra restrictive caps on the variety of remedy periods per 12 months or the size of a keep at an inpatient facility.
The federal Psychological Well being Parity and Dependancy Fairness Act banned these more durable limits. So insurers shifted to a distinct option to deny care. “They’re not going to simply cowl limitless care, so that they need to do one thing to restrict utilization,” stated Tim Clement, the vice chairman of federal authorities affairs on the nonprofit group Psychological Well being America.
Insurers say they conduct what they name utilization evaluations, by which they will request and sift by remedy progress notes filled with delicate particulars, to evaluate whether or not suppliers are delivering applicable care. Nevertheless, suppliers, psychological well being care advocates and legislators have discovered that these evaluations are sometimes used as pretexts by insurers searching for a motive to dispute the need of remedy.
Lately, no less than 24 states have handed laws to attempt to regulate how insurers conduct evaluations of behavioral well being care.
After the New York legal professional common decided that insurers, together with EmblemHealth, Excellus and MVP, had violated state and federal legal guidelines with their evaluations, state legislators bolstered oversight of those processes in 2019. An Excellus spokesperson stated it had since adopted a number of reforms; MVP didn’t reply to ProPublica’s questions, and EmblemHealth forwarded a response from a managed well being plan commerce group known as the New York Well being Plan Affiliation, which stated that the state’s findings don’t replicate the business’s present practices. (Learn their full responses.)
The New York regulation requires insurers to depend on standards based mostly on proof and authorised by the state when scrutinizing care. Peer reviewers, who work for insurance coverage corporations to assess medical necessity or appropriateness of care, should be licensed suppliers with related experience in psychological well being. And relating to youngsters, insurers are usually prohibited from requiring preapproval for his or her psychological well being remedy or conducting evaluations in the course of the first two weeks of an inpatient keep.
Final 12 months, New York regulators discovered that Cigna’s and Wellfleet’s medical necessity standards had been out of compliance with the brand new regulation. The insurers are allowed to maintain working whereas they work with the state to convey their standards consistent with the regulation, in keeping with the state’s psychological well being workplace. (The businesses didn’t reply to requests for remark.)
A number of states, resembling Massachusetts, New Mexico and Hawaii, make insurers speak in confidence to sufferers and suppliers the factors or insurance policies that they depend on for evaluations.
Insurers normally choose the clinician conducting evaluations, however in Illinois, if there’s a disagreement concerning the necessity of a remedy, a affected person can go for one other scientific reviewer, collectively chosen by the affected person, their supplier and the insurer.
Some states have additionally restricted the frequency of evaluations. In Delaware, insurers are usually prohibited from reviewing inpatient substance use remedy within the first 14 days. In Kentucky and Ohio, for sufferers with autism, insurers can not request a couple of overview yearly for outpatient care.
What should insurers reveal about psychological well being care entry?
It may be exhausting to implement the legal guidelines requiring equitable protection for psychological and bodily circumstances; doing so entails evaluating very completely different sorts of well being care and efficiently arguing there may be an imbalance in entry. State and federal regulators even have minimal assets for such intensive examinations, which has hindered their capability to scrutinize insurers.
To carry insurers accountable, no less than 31 states and the District of Columbia have handed legal guidelines requiring them to report how a lot entry they actually present to psychological well being care.
Most of those states ask insurers to offer particulars on their remedy standards or limitations, however some states look like violating their very own legal guidelines by not posting data publicly.
New Jersey’s Division of Banking and Insurance coverage, for instance, should make an insurer grievance log publicly obtainable and put up an insurance coverage compliance report associated to psychological well being care. However no such data has been revealed on its web site greater than 5 years after the state handed this requirement.
After ProPublica requested concerning the lack of transparency, spokesperson Daybreak Thomas stated that the division is working to implement the necessities and that the reporting course of would start this 12 months. “We acknowledge that the reporting provisions within the regulation present necessary public perception into compliance of carriers,” she instructed ProPublica in an e mail.
Chris Aikin, a spokesperson for the unique invoice’s major sponsor, New Jersey Meeting Speaker Craig Coughlin, instructed ProPublica his workplace had been in touch with the division and would “monitor their progress to fulfill reporting necessities and guarantee full transparency for customers.”
For compliance reviews, states usually request knowledge and analyses from insurers, however the figures that insurers submit is probably not detailed and even correct.
“I’ve reviewed lots of these analyses,” stated Clement, who has helped advocate for larger insurer transparency in a number of states, “and in most states, they’re fairly unhealthy.”
However in some states, like Oregon, the place detailed annual reporting is required, analyses revealed a disproportionate variety of insurance coverage claims for behavioral well being had been out-of-network in contrast with medical claims, suggesting that folks might have confronted hassle accessing therapists coated by their insurance policy.
Its reviews additionally discovered that psychological well being suppliers had been paid considerably lower than medical suppliers for workplace visits of equal size. For an hourlong workplace go to, a psychological well being supplier was, on common, reimbursed about half the quantity given to a medical or surgical clinician. A spokesperson for the state’s Division of Shopper and Enterprise Companies instructed ProPublica that there have been no investigations or enforcement actions in response to the brand new necessities.
“There’s no means we are able to really feel assured that anybody is following the regulation until we be certain there may be accountability they usually need to show that they’re accountable,” Clement stated.
Different states, like New York, have begun to make use of the brand new knowledge to drive investigations. Since 2021, the state’s Division of Monetary Companies has carried out 9 investigations of seven insurance coverage corporations in response to the legal guidelines, in keeping with a division spokesperson.
Individuals can file complaints with their state insurance coverage departments in the event that they imagine that an insurer is violating their rights.
This story comes from ProPublica, a nonprofit newsroom that investigates abuses of energy.
Share your story: In case you have submitted a grievance to a state insurance coverage division that you simply want to share with ProPublica reporters, attain out at [email protected].
ProPublica reviewed legal guidelines and laws in all 50 states and the District of Columbia. In the event you see a state regulation that was not included, please ship them a observe.
Max Blau of ProPublica contributed analysis to this report. Maps by NPR’s Connie Hanzhang Jin.